The term “denial” in the healthcare world has two meanings.
First, the obvious. It’s a psychological term often used to describe a natural defense mechanism in which we ignore feeling unpleasant.
Second, it’s a term that’s best described as one of a medical organization’s worst nightmares. You see, the second meaning for denial in healthcare happens when an insurance organization doesn’t accept services rendered by a physician.
In other words, a denial in the medical billing space means that you aren’t getting paid.
Sure, you could say that I’m being a little melodramatic. After all, seasoned medical billing professionals will be the first to tell you that certain denials are less of something that you can avoid and more so an inevitability. They have a point.
Either way, they’re not called an “acceptance” by any means, so they’re still bad news.
There are thousands of different reasons for denials out there and equal if not more techniques to implement within your organization to prevent them. However, that piece creeps outside the scope of this particular blog post.
Since many professionals view them as an inevitable part of the medical billing landscape, what can you do when your office receives one?
After all, if you rendered service on a patient…your organization deserves to get paid. Yet, the medical claim denial landscape is grim for modern-day healthcare facilities. A recent study found that denial write-offs sit at an average of 53%.
A rate that high isn’t something that many organizations can afford, leaving smaller practices with a hard decision to make.
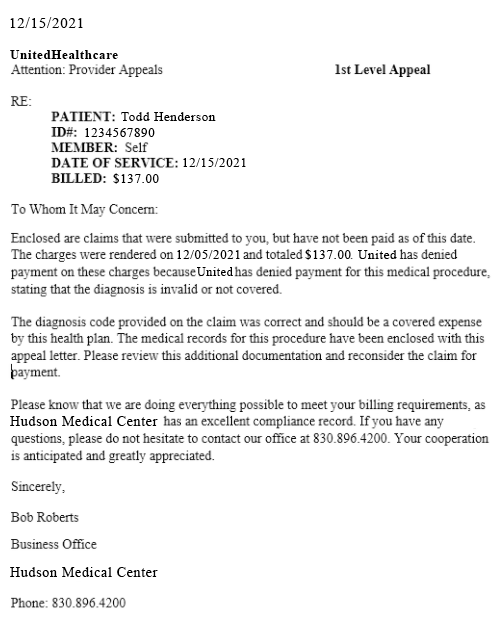
If you’re faced with that scenario you really only have one option to pursue, submit appeal letters.
The only question, though, is, “What should my appeal letter look like?”
Table of Contents
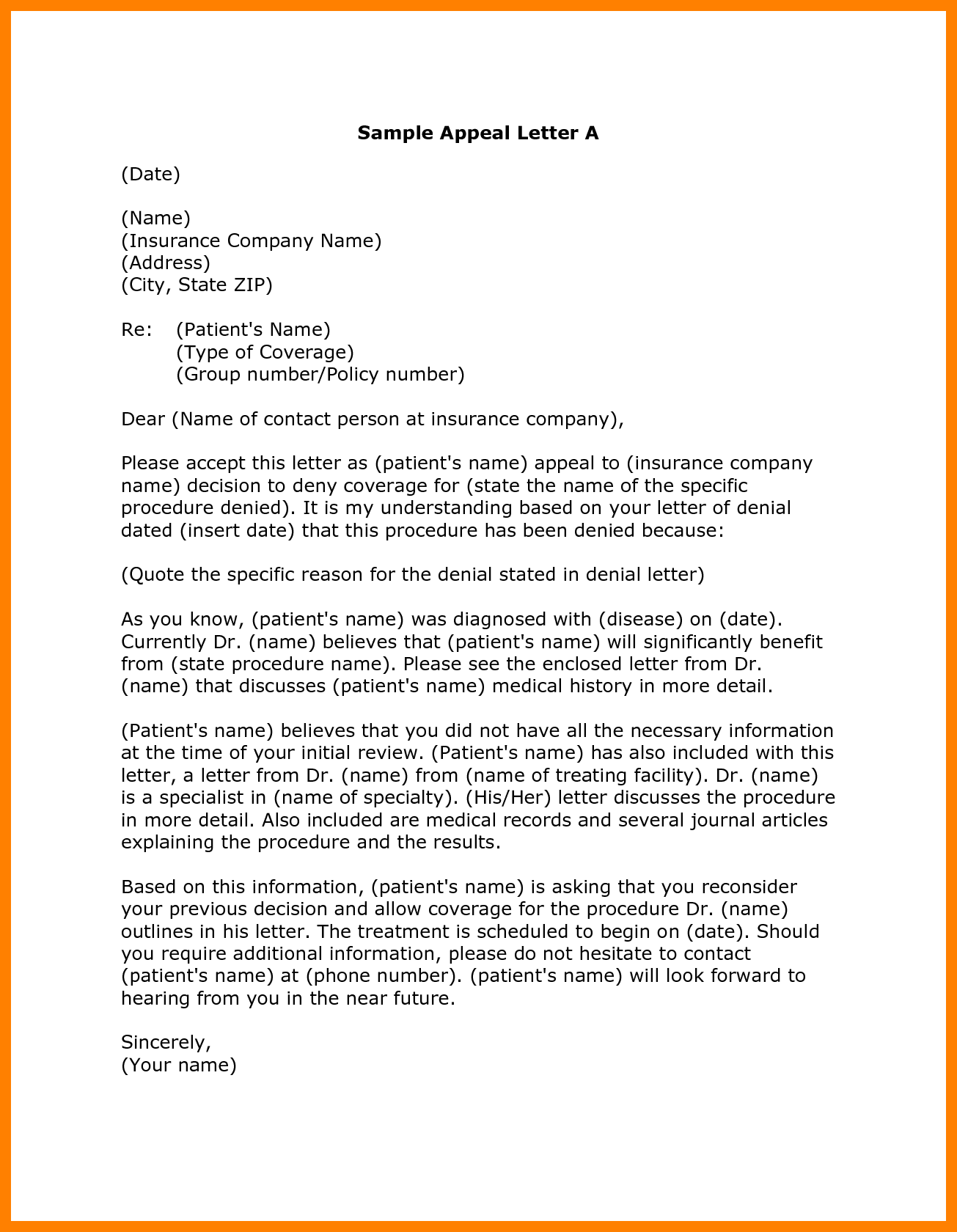
Sample 1: A Template for Time Savings
Not only are you at a disadvantage already from a statistical standpoint when it comes to medical claim denials but also from a time perspective as well.
You see, the majority of doctors already state that they need at least 50% more time with patients. No wonder burnout is ravaging the healthcare landscape.
In other words, that statistic proves that facilities don’t have time. And, if these organizations had more time, they would allot it toward their clients. I don’t blame them…that’s why these places exist.
Anyway, the point I’m trying to make with all of this is that although getting paid for a claim by an insurance provider helps keep the lights on, it doesn’t take precedence over client time.
All of this mess leads us to the statistic from earlier that pointed out the average rate of writing off claim denials.
So, if time is the leading factor as to why your organization doesn’t send appeal letters for your medical claim denials, what should you do?
You need to make a template appeal letter.
This first sample appeal letter from Mt Home Arts and is exactly that, a template. Every time you receive a medical claim denial, there’s data that you will always receive back, such as…
Insurance Provider
Claim Adjustment Reason Code (CARC)
Date of denial
Now, that isn’t that much data but it’s all you’ll need because you already have all of the additional information available.
Plug in what comes back from the insurance organization and the information you already know into your appeal letter template. Before you know it, you’ll have all of your denials ready for resubmission in half the time it took you prior to instituting a template.
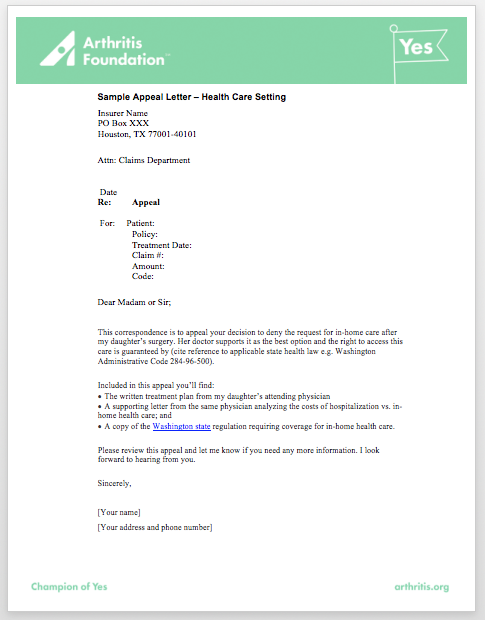
Sample 2: Incorporate Your Brand for Professionalism
For healthcare providers, branding is oftentimes an afterthought. I’m not trying to call you out if you fall within this majority, it goes back to what I stated earlier. Your number one priority is providing care for your clients.
Not to mention the fact that oftentimes a doctor’s name and title carries enough weight in most eyes to know that anything sent from them is important.
However, when it comes to sending appeal letters to insurance organizations…they’re all coming from doctor’s offices.
In other words, although being a doctor is a great achievement that leads to a certain level of respect, it’s not going to lend you any greater chances of your appeal letter having success.
All of this means that you need to figure out a way to make your letter stand out.
The best way to achieve this goal is by incorporating your brand throughout the document. This example from arthritis.org accomplishes that technique extremely well.
You see, having a professionally designed appeal letter that incorporates your organization’s logo and colors changes the entire dynamic of what you’re sending.
Likewise, the design and formatting of your entire letter matter.
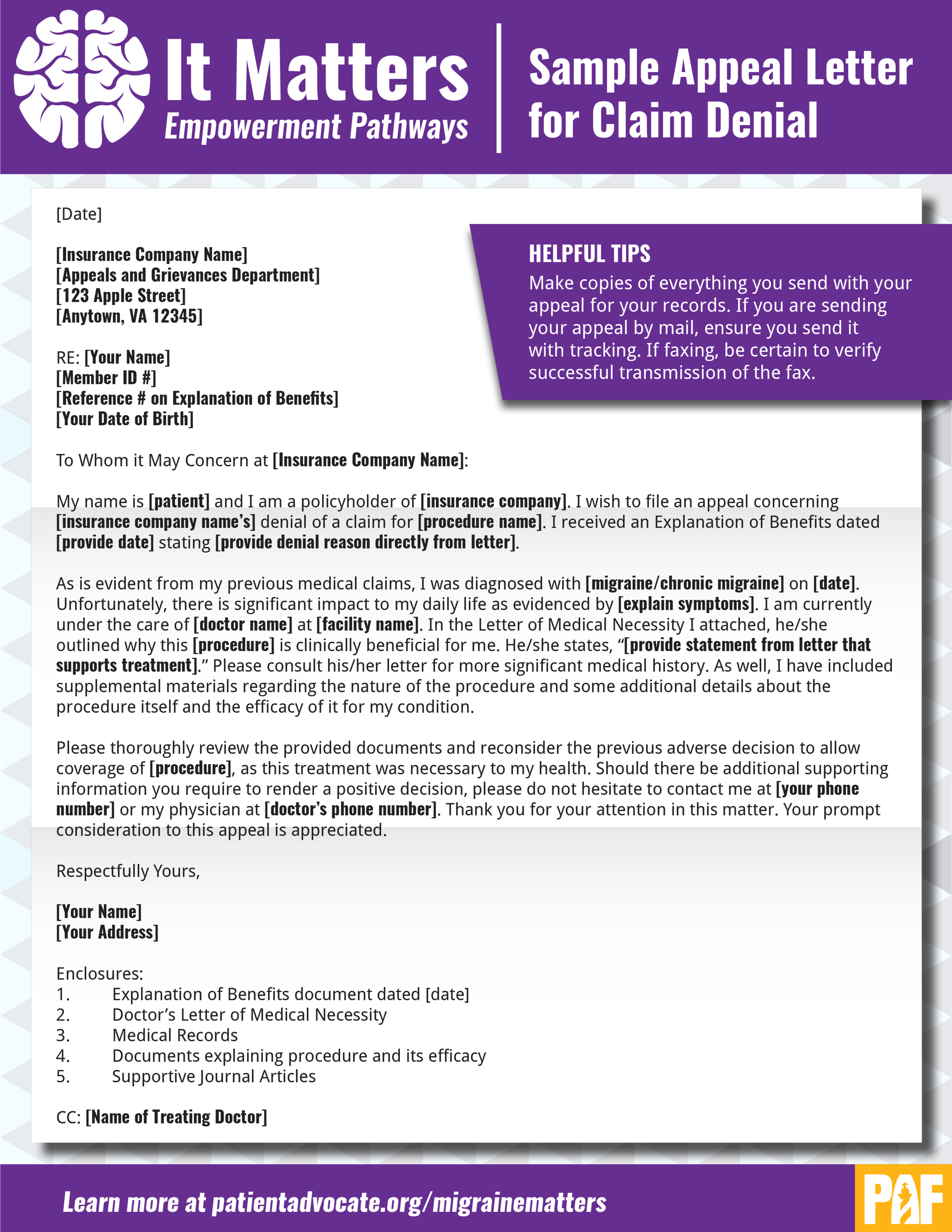
Sample 3: Keep Records and Tracking Information
If you’re manually sending your appeal letters, you need to make sure that you’re keeping a record.
That record should not only include a copy of what you sent, but also when you sent it and when it reached the insurance payer. The last part of the previous sentence is what’s most important.
Whether you’re sending your appeal letter through the mail or electronically, it’s imperative that you have tracking information.
This is such an important piece of the puzzle because it gives you a timeline glimpse into the process involved with trying to appeal a denied claim.
There’s also the harsh reality that is communicating with insurance providers. In a perfect world, as soon as an insurance provider receives an appeal letter, they respond to it and fix any mistakes that might have occurred.
Unfortunately, that’s not the reality. You may have to follow up multiple times with providers regarding your medical claim denials. But if you don’t keep records and/or don’t have tracking information on what you send, it makes the follow-up process much harder.
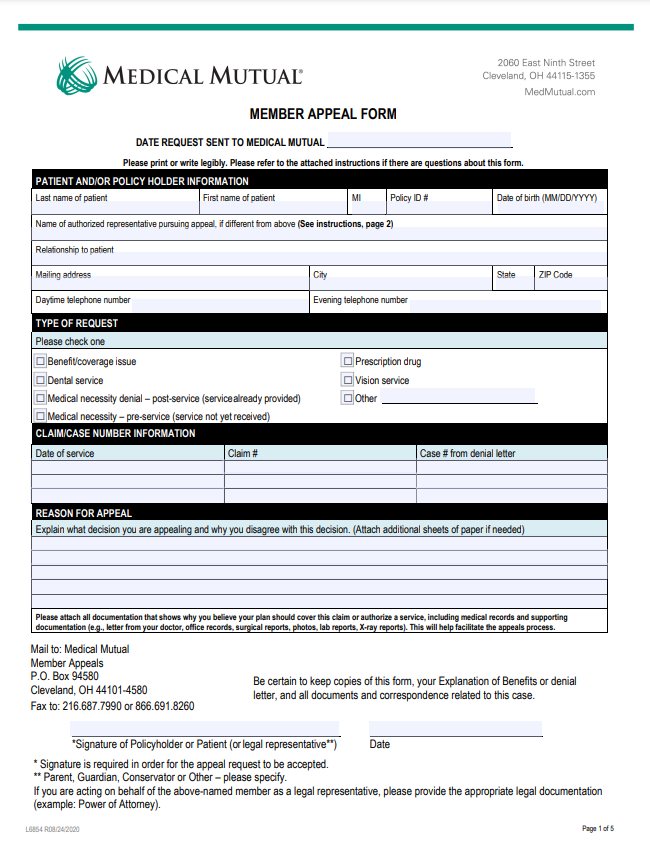
Sample 4: Insurance Provider Form
Since the insurance providers are the organizations who deny the medical claims that you submit, they have no choice but to have a standardized process put in place.
Thus, many of them allow for electronic submission…but only if you use the form that they provide.
The form provided above is just the first page in the appeal form provided by Medical Mutual.
It has everything going for it. It’s…
Templated
Branded
Using interactive forms
It even provides extra information about the insurance organization’s timely filing limit.
Maybe this is the golden sample. We can throw every other sample that I went over earlier in this blog post, right? Wrong.
You see, on a small scale sending filling out the electronic appeal letterforms that exist on insurance providers’ websites is attainable.
However, not every patient that comes through your doors seeking help uses Medical Mutual. I’d wager to bet that if ten of your patients walked through your door all at once, less than half of them would use the same insurance.
In other words, you and your staff can’t keep up with all of the different electronic appeal forms for every denial you receive…from all of the different insurance carriers your patients use.
Going this route is an option, but it’s not perfect.
Sample 5: Auto-Generation via Software
Alright, at this point you’ve seen multiple different sample appeal letters that you can use as the basis of creating your own.
Looking at the samples provided thus far will help you lessen the time it takes to resubmit your medical claim denials, no doubt.
But what if I told you that there’s a sample appeal letter type that can save you the most time?
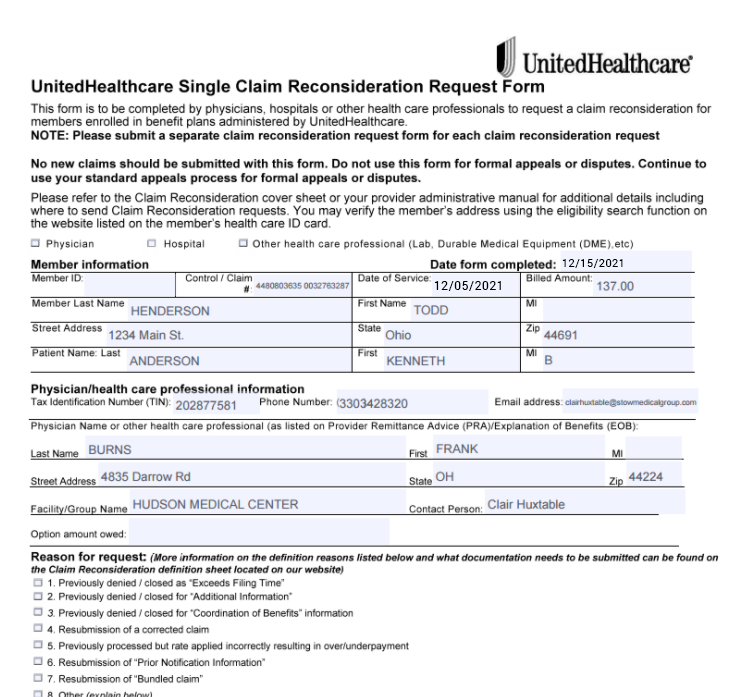
OK, I know what you’re thinking. The sample above is essentially the same form as the one from the previous section. You’re right, except for the fact that this one is for UnitedHealthcare instead of Medical Mutual.
The difference isn’t the form, it’s how the information gets appended to it.
You see, there are solutions out there that automatically pre-fill appeal forms, regardless of the insurance provider.
To make things even better, these solutions auto-generate an appeal letter as well.
Thus, you won’t have to worry about having a template, keeping records on tracking information and manually entering the information onto the insurance organization form. Although a solution like that costs money, it offsets its cost over time while also making you money in the long run.
Conclusion
By the end of this blog post, you’ve gone through a whirlwind of emotion. Although it’s worth looking into the different sample appeal letters for medical claim denials that are out there, they’re not the best option.
In order to truly tackle the mountain of denials that your organization deals with, you’re faced with two options.
First, you could be like the majority of healthcare practices and write off your denials as a loss in your books every year. Second, you could invest a little bit of money into a solution that streamlines your entire appeal letter submission process.
The second option helps you conquer your denial situation, leading to an overall increase in revenue for your organization.